
Most new parents have been warned about the potential risks of SIDS. There is still a lack of knowledge regarding the cause of SI DS which makes knowing how to prevent it difficult. Years of research have been poured into this topic, and recent updated recommendations were released by the American Academy of Pediatrics in 2022. Certain factors which are known to increase the risk of unexplained and explained (avoidable) SIDS have been identified.
The American Academy of Paediatrics (AAP) put forward the ABCs of Safe Sleep and the International La Leche League developed the Safe Sleep 7 to accommodate breastfeeding moms. There are fundamental differences between these two perspectives, which we will expand on in this article.
These safe sleep practices are not only intended to reduce the risk of SIDS but also prevent other sleep-related accidents. Whilst we understand that safe sleep is an emotional and controversial topic, we encourage parents to empower yourself with scientific evidence and research, in order to make informed decisions for your family.

What is sids?
SIDS is the main cause of death in babies between the ages of a month and a year with the rate peaking during the first 4 months of life. It is reported that over 90% of SIDS deaths occur before a baby reaches 6 months of age.
The American Academy of Pediatrics (AAP) defines Sudden Unexpected Infant Death (SUID) as a term to describe any sudden and unexpected death, whether explained or unexplained, occurring during the first year of a child’s life. After investigation, it may be determined that an unexpected death was caused by a specific unnatural or natural cause, such as:
- Suffocation,
- Asphyxiation,
- Entrapment,
- Infection,
- Ingestions,
- Diseases,
- or trauma (unintentional or nonaccidental).
Unexpected deaths that cannot be explained are referred to as sudden unexplained infant death.
To clarify; explained deaths would be attributed to a cause, whereas true SIDS is a completely unexplained cause of death.

HOW COMMON IS SUIDS IN SOUTH AFRICA?
A recent study concluded that “Africa may have the highest global rate of SIDS with a high burden of associated risk factors. SIDS and other sudden infant deaths accounted for between 2.5 to 21% of infant deaths in South Africa” (Godwin K Osei-Poku et al 2021)
Whilst the actual recorded SIDS rate is relatively low in South Africa, these statistics are grossly inaccurate. Due to limited resources and funding, underreporting to police services, unregistered births and poverty, there is very poor investigation, autopsy, medical history review, and appropriate laboratory testing done following the sudden death of a baby. Unless foul play is suspected, there is a high chance that the cause of death will not be investigated.
It is therefore entirely plausible that we indeed have a much higher prevalence of SIDS / SUIDS in South Africa.
what is the current thought behind sids?
The current train of thought as agreed upon by various researchers is that there are three factors, known as the Triple Risk Hypothesis, which contribute to a baby passing away from SIDS. This hypothesis suggests that when a baby who is vulnerable, such as a premature or low birth weight baby, is exposed to outside factors, such as sleeping on their tummy, during a critical period of time when their brain is not yet sufficiently developed to be able to control their heartbeat and breathing, then there is an increased chance of SIDS occurring. Adding to this is the difficulty a baby has with waking up from a deep sleep in order to respond to changes and increase their breathing or heart rate.
There is scientific research which shows that the major risk factors for SIDS, such as your baby sleeping on their tummy, sleeping on a soft mattress, maternal smoking, prematurity, low birth weight and potential head covering from loose items in their sleep space, have significant effects on their blood pressure and heart rate as well as their control over those functions. These major risk factors can also make it more difficult for them to wake up.

Triple Risk Hypothesis. (Adapted by the National Institutes of Health with permission from (87).)
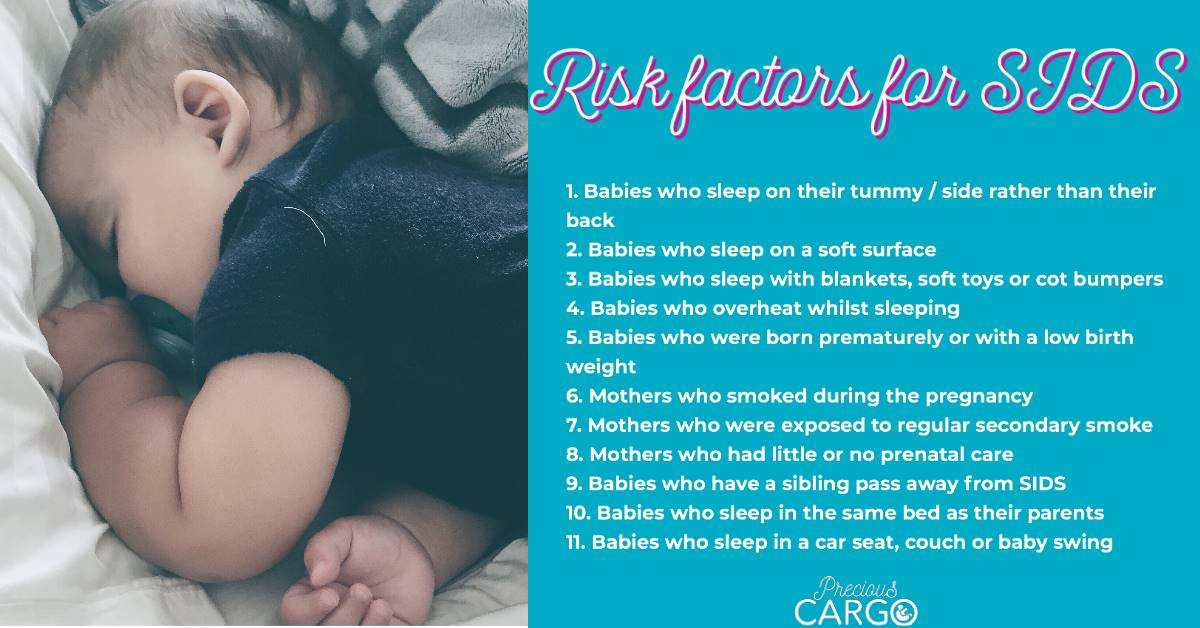
what are the risk factors of sids?
Although SIDS is not entirely preventable, the following risk factors increase the possibility of SIDS:
- Babies who sleep on their tummy or side rather than their back
- Babies who sleep on a soft surface
- Babies who sleep with blankets, soft toys or cot bumpers
- Babies who overheat whilst sleeping
- Babies who were born prematurely or with a low birth weight
- Mothers who smoked during the pregnancy (a SIDS related death is 3 times more likely to occur)
- Mothers who were exposed to secondary smoke from other members in the same house
- Mothers who had little or no prenatal care during their pregnancy
- Babies who have a sibling pass away from SIDS
- Babies who sleep in the same bed as their parents
- Babies who sleep in a car seat, couch or baby swing
what should sids not be confused with?
As important as knowing what SIDS is, the Safe to Sleep Campaign also indicates specific things that SIDS is not. SIDS should not be confused with the following:
- SIDS is not the same as suffocation and is not caused by suffocation.
- SIDS is not sleep apnoea
- SIDS is not caused by vaccines or immunizations
- SIDS is not contagious.
- SIDS is not the result of neglect or child abuse.
- SIDS is not caused by cots.
- SIDS is not caused by vomiting or choking
what other sleep-related causes of death are there?
Sudden Unexpected Infant Death Syndrome (SUIDS) is the term used to group all sudden and unexpected deaths during the first 12 months. SUIDS takes into account both deaths where the cause is unknown (such as SIDS) as well as those in which the cause is evident. Although SIDS accounts for the majority of infant deaths, other sleep-related infant injuries or deaths occur as a result of how and where your baby sleeps.
The Safe to Sleep Campaign mentions 3 types of possible injuries or mechanisms of death which fall under the SUIDS category and not SIDS:
- Suffocation can happen when a baby’s airway becomes covered and they are unable to get sufficient oxygen. This can result from soft bedding such as mattresses which are not firm enough, blankets, duvets, pillows or cot bumpers being placed in your baby’s sleep environment. It can also result from “overlaying”, which is when another person sharing the same sleeping surface as the baby accidentally rolls on top of or lays against them blocking the their breathing.
- Entrapment happens when your baby becomes trapped between two items such as a mattress and the side of the cot, wall or furniture. This can result in them getting stuck in a position in which their mouth or nose become covered and they cannot breathe.
- Strangulation occurs when something presses on or gets wrapped around your baby’s head and neck and closes off their airway making it difficult for them to breathe.

In order to minimise the chance of SIDS and other sleep-related deaths from occurring, safe sleep practices were introduced. Since these practices were established, the number of SIDS deaths has dropped dramatically. Overall, SIDS rates have declined by almost 75% since 1994 when the implementation of the “Safe to Sleep” campaign (formerly known as the “Back to Sleep” campaign) was launched. However, in 2019, SIDS, unknown or unexplained cause, and accidental suffocation and strangulation in bed were the second, third, and fourth most common causes of overall infant mortality. SIDS remains the leading cause of postneonatal death.

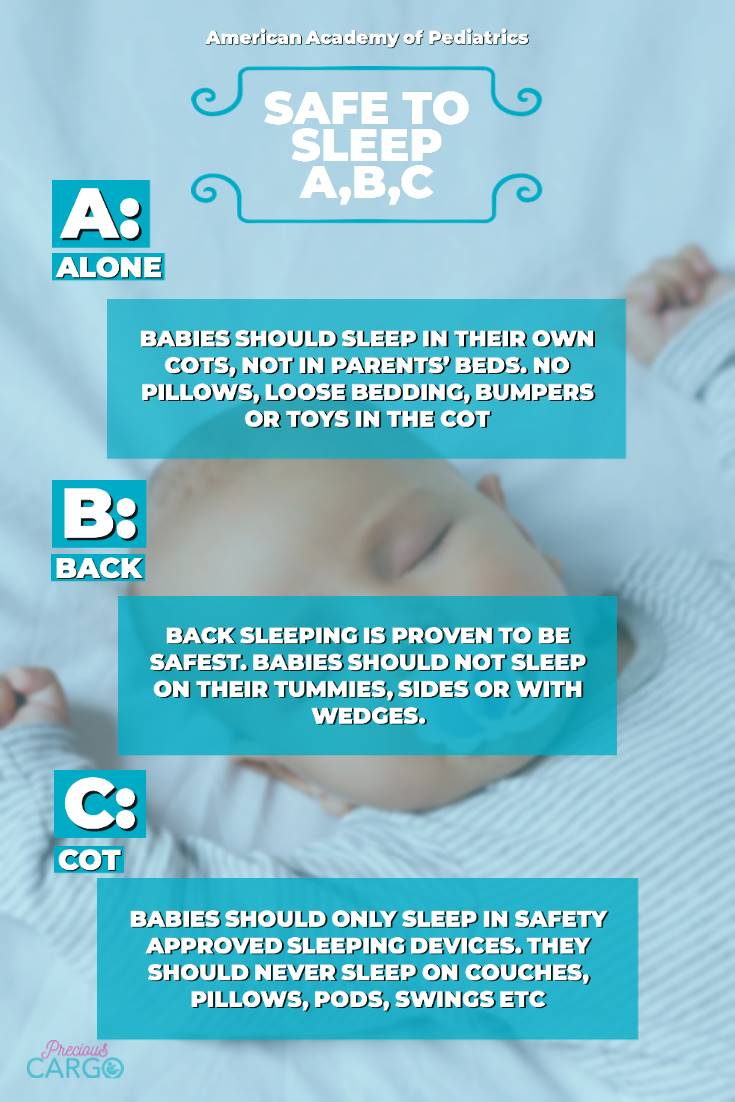
What are the American ACADEMy of PediatriC’s ABC’s of safe sleep?
The introduction of the Safe to Sleep Campaign assisted in dramatically decreasing the number of babies lost to SIDS. Initially, their main drive was “Back to Sleep” and encouraged parent’s to place their babies on their backs when sleeping as this is proven to be safest. It was later expanded to the ABC’s of safe sleep.
Your baby should always be
Alone, on their Back and in their Cot.
A is for alone
The AAP encourages sharing a room with your baby especially for the first 6 months, however sharing a room should not be confused with sharing a bed. Placing your baby to sleep on a separate surface such as a camp cot or Moses basket next to your bed is the safest place for them. It is also important that you do not fall asleep with your baby if you are on a couch or chair as this increases the risk of falls, suffocation, entrapment etc.
B is for back
The practice of placing your baby on their back for every nap and sleep has proven to reduce the risk of SIDS. The first thing that parent’s worry about when they hear this is the safest position for their baby to sleep is “won’t they choke if they vomit?”
Babies have an automatic reflex which allows them to cough or swallow anything that comes up which helps them keep their airway open. If they were to vomit while on their tummy or side, there is a far greater chance that they would breath in or suffocate as they may not be able to move their heads to open their airway.

c is for cot
In line with sleeping alone, your baby should sleep in their own cot with a mattress that is firm and flat as this helps reduce the chance of suffocation. Creating a safe sleeping environment also involves ensuring that there are no loose items such as duvets, blankets, pillows, sleep positioners or wedges, stuffed animals or bumpers as they also increase the risk of suffocation should your baby accidentally roll into them.
The safest cot for your baby is one that is empty, with only a firm, properly fitted mattress and fitted waterproof sheet. This includes not using any type of sleep positioners, inclined sleepers or wedges as they pose a large danger should your baby roll around while in one.
The updated AAP recommendations from 2022
- Nothing should be IN or NEAR the sleep space
- Babies should be placed on their backs for every sleep
- Use a safety approved bassinet, cot, Campcot or Moses basket with a FIRM mattress & fitted sheet
- Room share (but NOT bedshare) for the first 6 months
- Dummies are found to be protective against SIDS
- Breastmilk is considered protective against SIDS, if possible
- Immunisations are not a risk factor for SIDS
- Discontinue swaddling when baby shows signs of rolling
- If your baby falls asleep in a car seat, swing, pram, bouncer etc. they should be moved to a safe sleep surface as soon as possible
- Dress baby suitably for the temperature to avoid overheating
- Do not use weighted sleepwear
- Do not use hats when sleeping
- Inclined sleepers and wedges are not safe
- Insufficient evidence for AAP to fully recommend them, but parents can choose to use a bedside sleeper (if it passes the relevant safety standards)
- Babies should be doing regular, supervised, awake tummy time
- Despite their being no data on their safety, cradle boxes (cardboard boxes) may be considered culturally appropriate sleep spaces as long as baby is not bundled.

What are the Safe 7?
The International La Leche League indicates that although most breastfeeding moms do not plan on sharing their bed with their baby, ultimately 60-75% will at some stage do so. While they acknowledge that this is not in line with most safe sleep practices, they also recognise the benefits that are associated with sharing a bed. Those who do so report that they get more sleep and experience positive benefits on their milk supply. But is this recommendation proven to be safe?
To make this practice as safe as possible, they developed the Safe 7:
- You should be a non-smoker.
- You should be sober and unimpaired by any type of medication or drugs.
- You should be breastfeeding.
- Your baby should be healthy and full-term.
- Your baby should be on their back.
- Your baby should be lightly dressed.
- Both of you should be on a safe surface.

The last point of the Safe 7 indicates that you and your baby should be on a safe surface. To ensure this, they have pointed out 3 areas which should be checked:
- Avoid these items as they can be a potential smothering risk:
- Couches, chairs or recliners.
- A soft or sagging mattress that could cause your baby to roll into you or prevent them from lifting their head to a safer place.
- Avoid spaces where your baby may get stuck such as spaces between mattresses, headboards and walls.
- Pets which sleep on the bed.
- Make sure your bed does not have any:
- Unused pillows
- Heavy blankets or duvets
- Stuffed toys
- Any items such as cords or strings nearby
- Check your bed for potential hazards:
- The distance from the bed to the floor.
- The landing surface i.e. carpet or tiles or side tables.
- Anything that is sharp or could poke or pinch.
The International La Leche League claims that should you meet these 7 criteria, your baby is at no greater risk of SIDS than if they were sleeping in a nearby cot. At the time of publishing, we could not find any statistics or scientific evidence to verify this claim. In fact, there are several reported cases where babies have died despite parents following the Safe 7 guidelines.
What does the evidence suggest about bedsharing?
The AAP understands and respects that many parents choose to routinely bed share for a variety of reasons, including: facilitation of breastfeeding, cultural preferences, and belief that it is better and safer for their infant.
However, based on the evidence, the AAP are unable to recommend bed sharing under any circumstances. They recommend having your baby close by your bedside in a crib or bassinet will allow you to feed, comfort, and respond to your baby’s needs at night.
The AAP also stress that it is also important for parents, doctors, midwives, lactation consultants and other medical staff to know that the following factors increase the magnitude of risk when bed sharing:
More than 10 times the baseline risk of parent–infant bed sharing:
- Bed sharing with someone who is impaired in their alertness or ability to arouse because of fatigue or use of sedating medications (e.g., certain antidepressants, pain medications) or substances (e.g. alcohol, illicit drugs).
- Bed sharing with a current smoker (even if the smoker does not smoke in bed) or if the pregnant parent smoked during pregnancy.
- Bed sharing on a soft surface, such as a waterbed, old mattress, sofa, couch, or armchair.
- Term, normal weight infant aged <4 months old, even if neither parent smokes and even if the infant is breastfed. This is a particularly vulnerable time, so parents who choose to feed their infants aged <4 months old in bed need to be especially vigilant to avoid falling asleep.
- Bed sharing with anyone who is not the infant’s parent, including nonparental caregivers and other children.
- Preterm or low birth weight infant, even if neither parent smokes.
- Bed sharing with soft bedding accessories, such as pillows or blankets.
Which method is safest?
Although both the AAP and La Leche League both agree that the safest position for your baby to sleep is on their back on a firm mattress with no loose items around them, the AAP and La Leche League are in direct conflict in their views.
The AAP strongly discourages bedsharing/co-sleeping under any circumstances, while the La Leche League believe it is safe to do so if their above recommendations are adhered to.
It is important to note that co-sleeping while breastfeeding has been proven to increase the risk of your baby being smothered against your body, if you were to fall asleep. Read our article on how to sleep safer whilst breastfeeding.
Conclusion

From the available research and scientific evidence, there is significant evidence that shows the effectiveness of the Safe Sleep ABCs by The American Academy of Pediatrics in reducing the rate of SIDS and SUIDS occurrence. In contrast, there is no scientific evidence to support that the Safe 7 principles as being safe and risk-free. Although there are guidelines from La Leche League on how to bedshare as safely as possible, there is still noted risk involved.
Being informed of the benefits and risks of both methods and aware of how to make it as safe as possible, empowers you to make the safest, fully informed decisions for your baby. This goes a long way in reducing the risk of SIDS or any other sleep-related injuries or death.
Resources
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8719309/
https://www.ncbi.nlm.nih.gov/books/NBK513386/
https://safetosleep.nichd.nih.gov/safesleepbasics/SIDS
https://www.lullabytrust.org.uk/professionals/statistics-on-sids/
https://safetosleep.nichd.nih.gov/safesleepbasics/SIDS/fastfacts
https://www.mediclinicinfohub.co.za/sudden-infant-death-syndrome-sids/
https://pathways.org/abcs-of-safe-sleep/
https://www.llli.org/the-safe-sleep-seven/
https://www.healthychildren.org/English/ages-stages/baby/sleep/Pages/Safe-Sleep-Charlies-Story.aspx
https://www.sleepinglittles.com/blog/the-abcs-of-safe-sleep-what-does-it-mean
